You have reviewed a 45 year old quadriplegic who has a background history of Autonomic dysfunction.
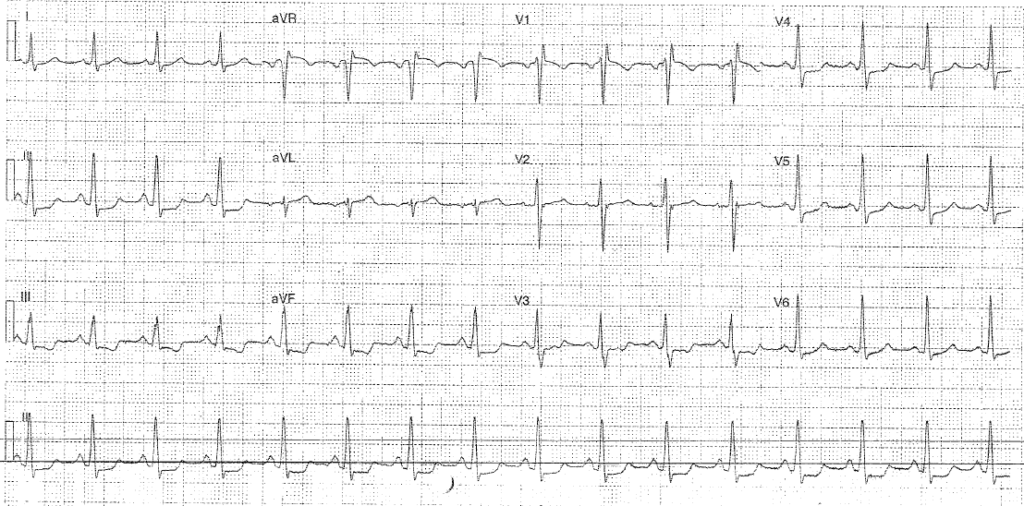
He took GTN at home after having a headache without checking his blood pressure and was brought in by his carer (feeling better) after recognising his systolic BP was 70 after GTN. On assessment his obs are P90 BP 111/77 RR18 Sats 98% air T37.7. He has had a cough for 2 months but his chest is clear on auscultation. His catheter is draining freely and abdomen is soft. There are no signs of cellulitis or pressure areas. He feels well. ECG is below:
How would you manage the patient?
He later drops his BP to 90-100 systolic which responds to 1L N saline and then remains stable. After several hours, whilst awaiting investigations, he also develops an oxygen requirement (requiring 4L n/s) How does this change your management?