ou have reviewed a 45 year old quadriplegic who has a background history of Autonomic dysfunction.
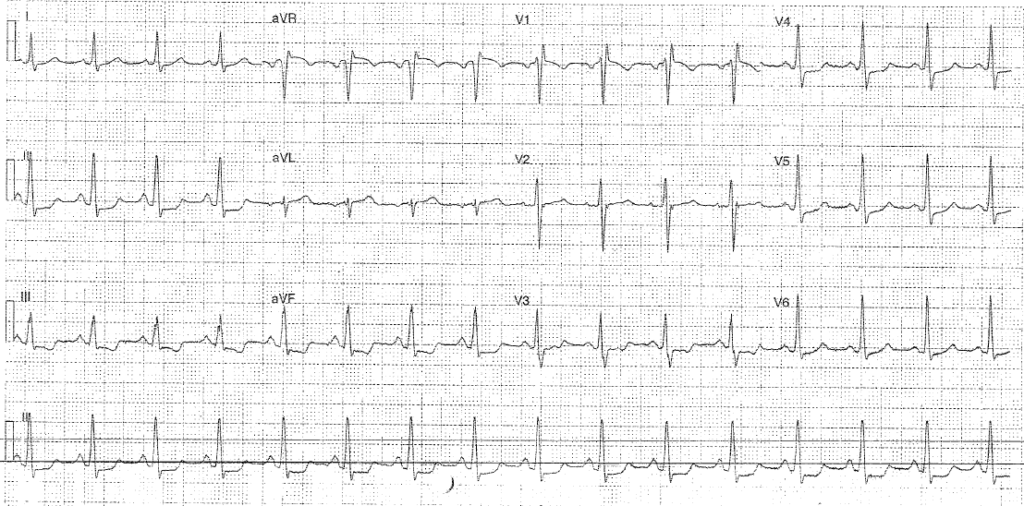
He took GTN at home after having a headache without checking his blood pressure and was brought in by his carer (feeling better) after recognising his systolic BP was 70 after GTN. On assessment his obs are P90 BP 111/77 RR18 Sats 98% air T37.7. He has had a cough for 2 months but his chest is clear on auscultation. His catheter is draining freely and abdomen is soft. There are no signs of cellulitis or pressure areas. He feels well. ECG is below:
- Rate: 96
- Rhythm: NSR
- Axis: Normal (0-90)
- Morphology: Widespread inferolateral STD 1-2mm, PR depression, RSR pattern V1, STE 1mm aVR
- Intervals: PR130 QRS 110 QTc 425
- Summary: Suggestive of LMCA occlusion
Typical findings in LMCA occlusion:
- Widespread horizontal ST depression, most prominent in leads I, II and V4-6
- ST elevation in aVR ≥ 1mm
- ST elevation in aVR ≥ V1
STE in aVR also seen in:
- diffuse subendocardial ischaemia eg O2 supply / demand mismatch
- proximal LAD occlusion
- tripple vessel disease
How would you manage the patient?
- Given low grade fever look for signs of infection (UA, CXR, FBC, CRP)
- Troponin (?myocarditis ?MI)
- Consider fluids if further episodes of hypotension
- Early cardiology involvement (in JHC MI equivalents are d/w the cardiology consultant)
Results
- UA was +ve (leu/nit) – commenced on IV ABx for same
- CXR was normal
- Trop was 240 (repeat 560)
He later drops his BP to 90-100 systolic which responds to 1L N saline and then remains stable. After several hours, whilst awaiting investigations, he also develops an oxygen requirement (requiring 4L n/s) How does this change your management?
- Nil to find on repeat chest exam (no sign of iatrogenic overload)
- We considered PE as diagnosis given the urine sample was from a catheter, the fever was low grade, and the patient was immobile given his history.
- CTPA showed large saddle embolus.
- He was admitted to ICU after d/w cardiothoracics (who felt him an unsuitable candidate for clot retrieval with co-morbidities)
- Considered as a candidate for thrombolysis
Further Reading – Textbook:
Chan TC, Brady WJ, Harrigan RA, Ornato JP, Rosen P. ECG in Emergency Medicine and Acute Care. Elsevier Mosby 2005.