Thank you for those that participated in today’s Simulation.
Case Summary:
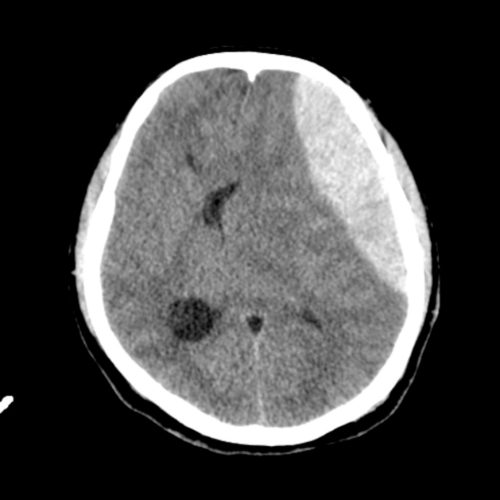
42yo man, fall from 3m height with head, facial and pelvic trauma. Initial GCS 12 with hemodynamic instability. GCS reduced further with unequal pupils requiring intubation, neuro-protective measures and transfer to trauma center for definitive neurosurgical care.
Learning Outcomes:
- Clear role allocation and team leadership.
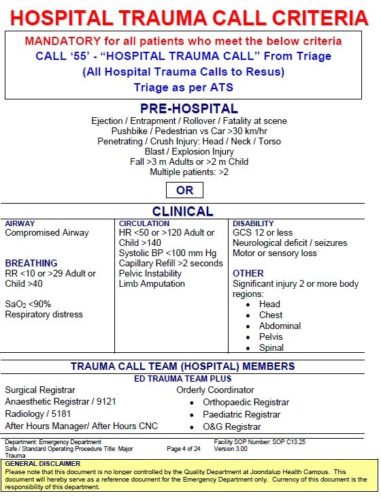
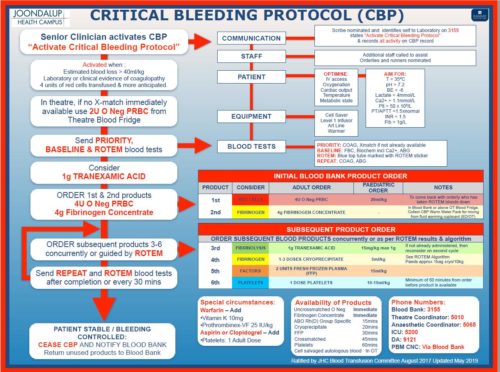
- Activation of hospital wide trauma call and Critical Bleeding protocol.
- Structured primary survey. Focusing on potential bleeding sources for trauma patient- external, chest, abdominal and pelvic cavities, long bone fractures.
Discussion Points:
Circulation control:
- Pelvic binding.
- Splinting long bone fractures.
- Tranexamic acid 1g- Must be given early, within 3 hours of injury.
- Early blood “replacing like with like” and MTP blood products.
- Source control- Theatre or interventional radiology for pelvic trauma.
Neuroprotective measures:
- Aim to minimise secondary brain injury by optimising cerebral blood flow. CPP=MAP-ICP
- Avoid hypoxia, hypercarbia, hypotension. Target etCO2 35-40mmHg.Maintain normothermia, normoglycaemia.
- Tilt bed to 30 degrees, remove neck constriction (remove Cspine collar and use midline in-line stabilisation).
- Intubation with modified RSI. Ketamine is an appropriate induction agent in multi-trauma. (see LITFL Neurocritical Intubation).
- Treat cerebral oedema- Hypertonic saline (more rapid onset) or mannitol.
- Definitive treatment of traumatic intracranial haemorrhage.
Challenges of managing trauma in Peripheral EDs
We discussed the timing of CT imaging and transfer of an unstable trauma patient with potential intracranial bleed. This would need to be discussed on an individual basis with RPH Trauma team and Neurosurgeons. A pan-CT scan may be considered at JHC as this will identify injuries and help plan surgery. However, CT should not cause delays in transfer and the patient receiving definitive care. Emergency burr-hole is not performed regularly by surgeons at JHC so should be deferred until neurosurgeons available.
For further information refer to JHC Major Trauma SOP